Eczema & Dermatitis
If you have eczema or dermatitis, it can have a real impact on your quality of life. Not only do these chronic conditions cause itching, pain and disrupted sleep, they can also stop you from taking part in a range of activities and making the most of daily life. We understand just how tough this can be. Luckily, there are some great treatments that can help control your symptoms and dramatically improve your quality of life. From non-prescription emollients and bath additives to steroid creams and ointments, we can help you find the best treatment for your skin and support you in effectively managing your condition.
Eczema & Dermatitis Treatments
 Fucibet Cream - Dual-Action Treatment For Infected Eczema£12.49
Fucibet Cream - Dual-Action Treatment For Infected Eczema£12.49
Fucidin Cream
Fucidin Cream - Fusidic Acid Antibiotic£9.99- Best seller

Betnovate Cream & Ointment
Betnovate Cream & Ointment (30g & 100g)£15.99 
Betnovate Scalp Application 100ml
Betnovate Scalp Application 100ml£15.99
Eumovate Cream & Ointment
Eumovate Cream & Ointment£15.99
Elocon Cream & Ointment
Elocon Cream & Ointment£14.49
Betamethasone 0.1% Cream & Ointment
Betamethasone 0.1% Cream & Ointment£15.99
Fucidin H Cream
Fucidin H Cream£15.99
Dermol 500 Lotion
Dermol 500 Lotion£8.99
Betacap 0.1% Solution
Betacap 0.1% Solution£17.99
Hydrocortisone
Hydrocortisone 1% Cream & Ointment£15.99
Trimovate Cream
Trimovate Cream£30.99
Cetraben Cream & Ointment
Cetraben Cream & Ointment£8.99
Elocon Scalp Lotion
Elocon Scalp Lotion£22.49
Dermol 200 Shower Emollient
Dermol 200 Shower Emollient£5.99
Mometasone Cream & Ointment
Mometasone Cream & Ointment£13.99
Dermol Cream
Dermol Cream£10.99
Fusidic Acid Cream
Fusidic Acid Cream£8.99
Betnovate RD Cream
Betnovate RD Cream£21.99
Doublebase Gel
Doublebase Gel£9.99
Epimax Cream
Epimax Original Cream£4.39
Eumovate
Eumovate Eczema & Dermatitis Cream£7.99
E45 Itch Relief Cream
E45 Itch Relief Cream£9.99
HC45 Hydrocortisone Cream
HC45 Hydrocortisone Cream£6.69
Sebco Ointment
Sebco Ointment£22.99
Epaderm
Epaderm Cream and Ointment£9.99- Best seller

Adex Gel
Adex Gel£9.99 
Clobetasone 0.05% Ointment
Clobetasone 0.05% Ointment£15.49
Diprobase Cream
Diprobase Advance Eczema Cream£11.99
Dermol 600 Bath Emollient
Dermol 600 Bath Emollient£10.99
Polytar Shampoo
Polytar Shampoo£10.99
Eurax Cream
Eurax Cream£8.99
E45 Cream
E45 Cream£14.49
Betnovate Lotion
Betnovate Lotion£15.99
Balneum Intensiv Cream
Balneum Intensiv Cream£14.00
Nystaform HC
Nystaform HC£19.99
Eurax HC Cream
Eurax HC Cream£5.99
Doublebase Dayleve Gel
Doublebase Dayleve Gel£9.99
Balneum Plus Cream
Balneum Plus Cream£24.99
Hibiwash
Hibiwash Skin Cleanser£10.99
Aveeno Cream
Aveeno Cream£9.99
Dermacool 2% Menthol Aqueous Cream
Dermacool 2% Menthol Aqueous Cream£24.99
Eucerin 10% Cream
Eucerin 10% Urea Cream£9.99
CeraVe Moisturising Cream
CeraVe Moisturising Cream£8.99
Aveeno Daily Moisturising Lotion
Aveeno Daily Moisturising Lotion£6.49
CeraVe SA Smoothing Cleanser
CeraVe SA Smoothing Cleanser£22.49
Doublebase Flare Relief
Doublebase Flare Relief£16.75
CeraVe Moisturising Lotion
CeraVe Moisturising Lotion£15.99
CeraVe Reparative Hand Cream
CeraVe Reparative Hand Cream£6.49
Oilatum Cream
Oilatum Cream£13.99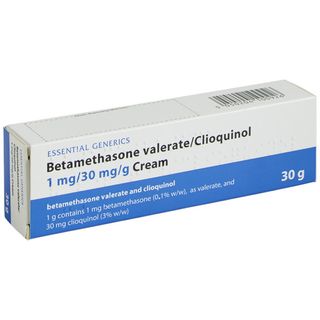
Betamethasone with Clioquinol Cream
Betamethasone with Clioquinol Cream£49.99
Aveeno Dermexa Cream
Aveeno Dermexa Cream£10.99
CeraVe AM Lotion
CeraVe AM Facial Moisturising Lotion£14.99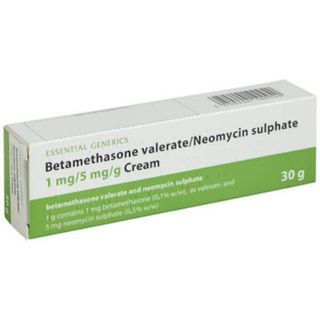
Betamethasone with Neomycin Cream
Betamethasone with Neomycin Cream£49.99
CeraVe PM Facial Moisturising Lotion
CeraVe PM Facial Moisturising Lotion£14.99
Aveeno Skin Relief Soothing Shampoo
Aveeno Skin Relief Soothing Shampoo£9.79
CeraVe Eye Repair Cream
CeraVe Eye Repair Cream£13.49
CeraVe Blemish Control Gel
CeraVe Blemish Control Gel£13.49- New product
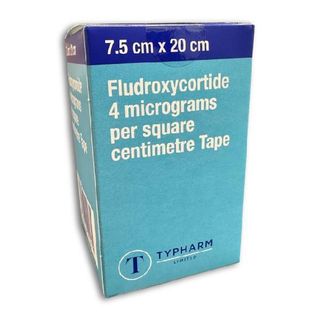
Fludroxycortide Tape
Fludroxycortide Tape£34.99 
Xepin 5% Cream
Xepin 5% Cream - Relief From Eczema Itching£29.99
CeraVe SA Renewing Foot Cream
CeraVe SA Renewing Foot Cream£8.99
CeraVe Hydrating Cleanser
CeraVe Hydrating Cleanser£16.99
Dermax Therapeutic Shampoo
Dermax Therapeutic Shampoo£9.79
CeraVe SA Smoothing Cream
CeraVe SA Smoothing Cream 10% Urea£14.99
CeraVe Foaming Cleanser
CeraVe Foaming Cleanser£16.99
CeraVe Hydrating Hyaluronic Acid Serum
CeraVe Hydrating Hyaluronic Acid Serum£19.99
CeraVe Hydrating Cream-to-Foam Cleanser
CeraVe Hydrating Cream-to-Foam Cleanser£13.49
CeraVe Hydrating Foaming Oil Cleanser
CeraVe Hydrating Foaming Oil Cleanser£12.99
Nystaform Cream
Nystaform Cream£19.99- Out Of Stock
E45 Eczema Repair Cream
E45 Eczema Repair Cream£10.90 - Out Of Stock

CeraVe Micellar Cleansing Water
CeraVe Micellar Cleansing Water£10.99
Start your assessment for Eczema & Dermatitis
Don't wait to get the medical help you need.
Once you complete a short online assessment about your condition, you will be able to select your preferred treatment and quantity from a list of appropriate options for you.
- Reviewed by our UK-based medical team
- Takes less than 3 minutes to complete
- Approved treatments dispatched same day (before 3pm)
Ordering as easy as 1, 2, 3
1. Find the ideal treatment
2. Get a free consultation
3. Enjoy speedy delivery
Advice for Eczema & Dermatitis
What is Eczema?
If you’ve been wondering where to buy eczema and dermatitis treatment when you need it most, then congratulations, you’ve found the right place. Here at the Independent Pharmacy, we stock eczema cream, ointment, shower emollient and more to aid your treatment and relief from the painful itching that dermatitis causes.
A discreet, reliable service, we will ship your products direct to your preferred address when you purchase online with our trusted pharmacists. We will provide guidance on the best eczema remedy for you and ensure that your order is fulfilled as quickly as possible. You won’t find medicated eczema cream or ointment cheaper anywhere else, start an online consultation today with The Independent Pharmacy to get your condition under control and relieve the symptoms of dermatitis.
Eczema is a long-term condition that affects the skin. It can also be referred to as dermatitis. Mild cases of eczema will cause the skin to become dry and itchy. It may also become scaly and red, and resemble a rash. In more severe cases of eczema, the skin may present with crusting, weeping or bleeding.
Eczema is a common skin condition affecting approximately one in every five children. The condition is slightly less common in adults, only affecting one in every twelve. As these statistics suggest, a significant number of children will ‘grow out’ of eczema during their teenage years.
The skin on our bodies is designed to provide a protective barrier against irritants and infections. It consists of three layers; a thin outer layer (epidermis), an elastic middle layer (dermis) and a fatty inner layer (hypodermis). All three layers contain skin cells, water and fats that help maintain and protect the condition of the skin.
Someone who suffers with eczema may not produce sufficient fats and oils to properly maintain these skin layers. This will also reduce the skin’s ability to retain water, causing the skin cells to become dry and cracked. This dryness can lead to tiny gaps opening up in the skin, making it easier for irritants and bacteria to penetrate its surface. It’s these irritants that cause the skin to become damaged, red and inflamed. This can lead to the sufferer scratching and splitting the skin open, causing it to bleed and leaving the wound open to infection.
What types of Eczema are there?
There are different types of eczema that can affect the sufferer in different ways:
Common types
Atopic Eczema: This is the most common form of eczema, characterised by red inflammation and bumps on the skin’s surface. It is primarily seen in children but can affect people of all ages. Fortunately, most kids will grow out of this type of eczema by their teenage years. The term ‘atopic’ refers to the fact that it generally has an unknown cause. These conditions are usually hereditary, although they are not always passed directly from parent to baby and may skip a generation.
Atopic eczema will present itself as an itch that chiefly affects the creases and folds of the body, such as the inside of the elbows, backs of knees and the hands. It is also known to affect the armpits, breasts, nipples, wrists, mouth, lips, neck, fingers and eyelids. This itch can become dry and red, with flare-ups occurring in small patches or all over the body. Spontaneous flare-ups are usually the result of an external trigger, the most common being: soaps, pollens, animal dander, overheating, house-dust mites, stress and harsh clothing.
Contact dermatitis: This is sometimes referred to as contact eczema. Contact dermatitis affects around 10% of the UK population making it the most common type of work related skin disease. This form of eczema can cause red, itchy and scaly skin that can sometimes sting and burn. It can lead to the skin becoming dry, cracked and blistered. Contact dermatitis can affect any part of the body, though the most commonly affected area tends to be the hands and knuckles.
Most cases of contact dermatitis are caused by the skin coming into contact with irritants, substances that physically damage the skin. Examples of these are detergents, soaps, antiseptics, perfumes and solvents. These irritants account for approximately eight out of ten cases of contact dermatitis. Another cause comes in the form of an allergen, which is a substance that causes the body’s immune system to react in a way that affects the skin.
Seborrhoeic eczema: This form of eczema affects the areas of the body that contain a large number of sebaceous glands, such as the scalp and the sides of the nose. It is characterised by a red rash or in case of the scalp; dandruff. It most commonly affects the scalp and face but it can spread to the centres of the chest and back. The armpits, under the breasts, groin, genitals and in between the buttocks can also be affected. The cause of seborrheic eczema isn’t fully understood. It is thought to be caused by a yeast known as pityrosporum ovale. This yeast is found on the skin of those affected by seborrheic eczema, however it is unclear whether the yeast is the sole cause or just a contributing factor to this form of dermatitis.
Less common types
Discoid eczema: This is sometimes referred to as nummular dermatitis and is usually found in adults with dry skin. This form of eczema presents as coin shaped discs of affected skin that are roughly the size of a two-pound coin. These discs have a slightly bumpy texture before they begin to ooze and crust over. The surface of the discs can then become scaly before the centre of the discs clears, leaving the skin dry and flaky. Discoid eczema will usually affect the lower legs, forearms or trunk. As with other forms of eczema the exact causes of nummular dermatitis is unclear. However, most sufferers presenting with the condition tend to have dry skin.
Gravitational eczema: This is sometimes referred to as varicose or stasis dermatitis. This form of eczema affects the lower legs and is more commonly experienced in later life. Poor circulation, blood clots and varicose veins put a person more at risk of developing this condition. Gravitation eczema will appear as dark red or brown patches under the outer layer of skin. As the condition progresses the skin becomes very thin and fragile and can easily break down, potentially causing an ulcer. In more severe cases the skin can start to weep, causing larger areas to crust over, leading to a varicose leg ulcer. This form of eczema is the result of poor circulation, which causes an increased pressure in the lower legs, leading to blood leaking through the very small vessels in the legs.
Asteatotic eczema: This is sometime referred to as eczema cracquele. This form of dermatitis will in most cases only affect those over the age of sixty years. Asteatotic eczema will present as small islands of dry rough skin clustered closely together. The appearance resembles ‘crazy paving’ with red and pink fissures or grooves separating each ‘slab’. Sufferers will experience soreness and itching in the affected areas. This type of eczema will initially occur on the shins but can be found on the upper arms, lower back and thighs as well. Asteatotic eczema is thought to be caused by a significant decrease in the oils on the skin’s surface. This may be the result of over cleansing or vigorous scrubbing. Low humidity can also contribute to developing the condition.
Pompholyx eczema: This can sometimes be referred to as dyshidrotic eczema. The main symptom of this form of eczema is a blistering that is confined to the hands and feet. These blisters are mainly found along the sides of the fingers and on the palms of the hand. In feet, they are predominantly found on the soles. The skin will be inflamed and feel very itchy. The blisters are prone to breaking and weeping with the skin beginning to peel as it starts to dry out.
How is Eczema diagnosed?
In most cases eczema and dermatitis can be easily diagnosed by your GP or pharmacist through a visual examination of the skin coupled with questions about your symptoms. Mainly they will want to know when the symptoms first appeared and what substances you have been exposed to. They will likely ask questions about your occupation and lifestyle in an attempt to identify what triggers or factors are causing your symptoms. Most common cases of eczema are not serious and symptoms can be kept under control.
If your GP is unable to diagnose eczema, they may refer you to a dermatologist. Seeing a dermatologist may also be necessary if your eczema has been successfully diagnosed but you are not responding to conventional treatment.
How is Eczema controlled and treated?
Treatment for eczema is split into two main categories:
- Emollients - regular use of moisturisers (up to four times daily) to keep skin moisturised and healthy
- Steroid creams - used in short courses to control flare-ups in eczema
Emollients
Emollients are moisturisers designed to keep the skin feeling hydrated, flexible and less itchy. One of the most important aspects of treating all types of eczema is keeping the skin soft and supple. This can be achieved by frequently applying generous amounts of emollients. Emollients are available in a variety of preparations, including; creams, ointments and lotions. If used on a daily basis, emollients effectively controls mild to moderate eczema.
Emollients, such as Dermol Cream, contain cleansing properties and are especially useful when used as a soap or shower gel substitute. Bubble baths, like soaps, can dry and irritate the skin. By using an emollient bath oil, such as Balneum Medicinal Bath Oil you can still cleanse, moisturise and indulge without the irritation. Emollients work best if applied directly after showering or bathing as water is still trapped in the skin. It is recommended that they be applied both generously and frequently (at least 3 - 4 times a day).
Emollient creams
Many people prefer using creams during the day as they feel lighter on the skin. However, all creams contain preservatives, which for some, can cause irritation over time. Examples of emollient creams include:
- Balneum & Balneum Plus Cream
- Dermol Cream
- Diprobase Cream
- Doublebase Gel
- E45 Cream
- Epaderm Cream
- Hydromol Cream
- Oilatum Cream
Emollient ointments
Unlike creams, ointments do not contain preservatives so are less likely to cause irritation. Ointments are by nature more greasy and for this reason many find them cosmetically unattractive. For this reason, many people use emollient ointments at night for intensive moisturising when the greasiness is less of an issue. It is not recommended to use ointments on weeping skin as ointments are effective at holding moisture, a cream or lotion is more appropriate in these circumstances. Ointment emollients are ideal for very dry and thickened skin. Examples of emollient ointments include:
- Diprobase Ointment
- Epaderm Ointment
- Hydromol Ointment
Emollient Lotions
The preparations are ideal for areas of the body that are hairy. They contain more water and less fat than creams so aren’t as effective as a moisturiser. Examples of emollient lotions include:
- Aveeno Lotion
- Dermol 500 Lotion
- E45 Lotion
Specially formulated products designed for use in shower and bath include:
- Hydromol Bath and Shower Emollient
- E45 Emollient Shower Cream
- Dermol 600 Bath Emollient
- Dermol 200 Shower Emollient
- Doublebase Emollient Shower Gel
- Doublebase Emollient Bath Additive
- Cetraben Emollient Bath Additive
- Balneum & Balneum Plus Antipruritic Medicinal Bath Oil
- Aveeno Body Wash
Topical Corticosteroids:
Topical corticosteroids refer to creams or ointments that contain steroids. When used as directed by your doctor or pharmacist, corticosteroids are one of the most effective treatments for eczema and dermatitis. Usually, a corticosteroid will be used if the skin has become very inflamed and red. These preparations are applied directly to the skin and work to rapidly reduce the inflammation. When using corticosteroids, a thin layer is applied to the affected area, usually no more than twice a day. For most cases, a single daily application will only be required.
There are varying types and strengths of topical corticosteroids, the appropriate selection will be made based on the severity of symptoms and where on the body they are located. Weaker corticosteroids are usually recommended for cases of mild eczema, or for the more sensitive areas of the body. A stronger corticosteroid will likely be recommended for use on the palms of the hands, knuckles or the soles of the feet and areas where the skin is thicker. If presenting with severe eczema or dermatitis, a strong corticosteroid may be prescribed for short-term use only. Examples of topical corticosteroids include:
Weaker preparations:
- Hydrocortisone Cream 1%
- Eumovate Cream (Clobetasone)
- Eumovate Ointment (Clobetasone)
Stronger preparations:
- Betnovate Cream (Betamethasone)
- Betnovate Ointment (Betamethasone)
Stronger preparations for the scalp:
- Betnovate Scalp Lotion (Betamethasone)
- Betacap (Betamethasone)
- Elocon Scalp Lotion (Mometasone)
Antibiotic preparations - only for use where infection is present:
- Fucibet Cream (Betamethasone & fusidic acid)
- Fucidin H Cream (Hydrocortisone & fusidic acid)
If the use of emollients and topical corticosteroids have proven ineffective at controlling your eczema, it may become necessary to seek alternatives treatments from a dermatologist.
Can I prevent flare-ups of Eczema?
There are many self-help ways in which eczema flare-ups can be reduced or prevented. Including:
- Use an appropriate emollient regularly to keep skin soft and moisturised.
- Avoiding exposure to extreme temperatures, such as very hot baths or showers.
- Avoid using harsh soaps, bubble baths and cosmetic products that can irritate the skin.
- After bathing or showering, pat areas dry with a soft cotton towel. This technique will leave a little moisture on the skin. By then applying a moisturising cream or lotion more moisture is locked into the skin.
- During the winter months use a humidifier. This will add moisture to the dry air experienced during the heating season.
- If contact dermatitis is the cause of your eczema flare-up, avoid contact with known triggers, such as detergents, cleaning solutions, other chemical irritants, jewellery, plants and any substance that triggers skin allergies.
Alternatives
Non-prescription alternatives for Eczema can include;
- Moisturisers and emollients
- Bath and shower gels
- Cotton gloves (to keep from scratching)
- Antihistamine tablets (to ease the itching)
FAQs for Eczema & Dermatitis
What are the different types of Eczema?
The name ‘eczema’ is given to a group of similar skin conditions which lead to dryness and irritation. There are a number of different forms:
- Atopic eczema – the most common type; though more common in children, it also affects adults
- Discoid eczema – occurs in circular patches on the surface of the skin
- Contact dermatitis – a reaction following contact of the skin with certain substance
- Varicose eczema – an eczema affecting the lower legs, resulting from poor blood flow
- Seborrhoeic eczema – characterised by discoloured, scaly patches on the nose, ears or scalp
- Dyshidrotic eczema – small blisters on the palms
What causes Eczema?
Eczema is a chronic skin condition whereby patches of skin become very dry and red- much like a rash. In some cases, and especially for kids, eczema will gradually improve over time. Eczema most frequently affects the knees, elbows, neck, face and hands.
Is Eczema contagious?
Eczema is not contagious.
Is Eczema hereditary?
People within a family often have similar susceptibilities to some skin conditions, including eczema. Eczema tends to develop concurrently with other hereditary conditions like hay fever and asthma.
How is Eczema diagnosed?
A doctor will usually be able to discern whether your skin condition is eczema or another similar condition. If normal eczema treatment does not provide relief, you may be referred to a dermatologist to identify the root cause of the condition. As eczema is often associated with an allergic response, you may be advised to have an allergy test. Common allergens linked to eczema symptoms include mites, fungal spores, pollen and some foods. In the case of food, certain changes may need to be made to the diet.
Does Eczema worsen with age?
Twenty percent of British children will develop atopic eczema to some extent. In the majority of cases, eczema will first develop while the child is a baby or toddler, and often in infancy.
Around half of children with eczema will see significant improvement by the age of eleven, and many will see the condition clear entirely by the time they reach adulthood. In some cases, however, eczema will remain through adulthood, or otherwise appear for the first time when the individual is an adult.
How can I find an Eczema specialist?
There is no medical specialty devoted to eczema; it falls under the umbrella of skin conditions, which are covered by dermatologists. A GP will refer you to a dermatologist if your eczema is particularly severe or if regular treatment is ineffective.
If you need help with a referral you can contact us and we will also be happy to help.
What will a dermatologist prescribe for Eczema?
Dermatologists will review your current medication and offer support to ensure that they are being used correctly. Further remedies they might offer include:
- Topical calcineurin inhibitors – these are ointments that will suppress your immune system, which include tacrolimus and pimecrolimus
- Topical corticosteroids
- Wet wraps or bandages
- Phototherapy – ultraviolet light which will combat further inflammation
- Immunosuppressants – tablets that work to suppress the immune system, which include ciclosporin, azathioprine and methotrexate
- Alitretinoin – medicine specifically for adults to treat severe eczema of the hands
- Psychological support if necessary
Are Eczema symptoms generally symmetrical?
Symmetrical symptoms usually indicate atopic eczema or psoriasis. Asymmetrical symptoms are typically due to causes from outside the body, like fungal infections or tinea.
Is it normal to have dry, flaky skin with Eczema?
This is normal – dry itchy skin is one of the characteristic symptoms of eczema.
What factors can trigger Eczema to worsen?
Many external factors can cause eczema to flare up. Though these will vary depending on the individual, common triggers will include:
- Allergens such as pollen, animal fur, mites, moulds, peanuts, eggs or soya. Reactions to lactose are very often associated with eczema
- Environmental factors such as dampness or dry weather
- Irritants in certain types of shampoo and cleaning products
- Contact with certain fabrics including wool and synthetics
- Hormonal changes in women, such as in the days preceding a period or whilst pregnant
- Stress
Your GP will counsel you on how to identify eczema triggers and how best to avoid them.
Is there a cure for Eczema?
As atopic eczema is a chronic condition, there is no cure. However, medication is effective at combating symptoms, and most children with eczema will find that their condition improves significantly with age.
What is the difference between creams, ointments, lotions? Which is the best one type use?
The best emollient is the one you use most often - the most important thing about emollient use is that it is regular (up to four times daily).
Different emollients can be used depending on your own routine - for example, a cream can be applied easily in the morning as it soaks in more quickly and an ointment can be applied at night as it is more greasy and takes longer to absorb.
Terminology is important in treating skin conditions, so here are the differences between the types of topical products:
A solution is a liquid with a base of water or alcohol. They are thin and easy to apply, but can cause further dryness for some people.
Lotions are slightly thicker than solutions. These can be used for large and/or hairy regions of skin.
Creams are thicker than lotions. They are used for smaller areas of skin, especially when a region is weeping.
An ointment is a product with high oil content. They can be greasy, and are used to treat dry and scaly skin.
For quite hairy parts of the body including the scalp, gels are used, which are more solidified. An alternative for the scalp is a mousse, a foamy product.
What treatments are there apart from emollients and steroids?
If your eczema does not respond to normal remedies, you may be prescribed topical treatments like tacrolimus or pimecrolimus. To combat itching, you can take antihistamines. If necessary, dermatologists might recommend more powerful treatments including special bandages to provide relief allow the skin to heal.
What is the best time to apply my Eczema treatment?
Emollients, such as Diprobase, Balneum and Cetraben, moisturise the skin and should be applied as often as necessary. This is normally two to four times daily depending on your routine and the severity of your eczema.
Special care should be taken to moisturise often, especially after washing, this will ensure the skin is protected from drying out. The skin absorbs moisturisers particularly well after washing so using emollients after showering or bathing is always a good idea. Washing the skin with soap, gels, shampoo or even very hot water can strip the skin of moisture and is not recommended.
Emollients can also be used in bath water and in the shower as a soap substitute.
Steroid creams, including Hydrocortisone, Betnovate and Eumovate, are applied as a think layer once or twice daily for a course of 7 - 10 days to treat a flare-up (always check the individual product instructions).
They should be applied in the morning and/or evening, leaving at least 15 minutes between applying your regular emollient and the steroid cream to allow both to absorb separately.
How much cream/ointment should I apply?
Emollients can be applied as often as you need them. As a general rule, you should always apply more emollient than you think - people tend to underestimate the amount of moisturiser required.
Application of steroid creams is measured in Finger Tip Units (FTU) - the amount of cream from the end of the finger to the first crease. Typically, one FTU would cover the equivalent area of skin of one hand.
What if I forget to apply my Eczema treatment?
Emollients can be applied as often as required. It is important to keep the skin hydrated so apply frequently and regularly. If you forget an application, apply at the earliest opportunity.
Thick emollient ointments sometimes block the hair follicles in the skin. This may cause a mild inflammation or infection of the affected hair follicles, which is called folliculitis. Ensure you apply emollients in the direction of hair growth after washing with shampoo to hep to prevent this.
If you forget to apply your steroid cream, apply the correct dose when you remember, and then carry on as before. If it is nearly time to apply the next dose, skip the current application and apply the next dose at the normal time.
Should I be worried about side effects?
The side effects of emollients are limited and minimal.
Over-the-counter creams and ointments can contain colors and perfumes. It is possible you may be sensitive to, or react to, these ingredients rather than the emollient itself.
Medical emollients don’t have colours or perfumes and are less likely to cause any irritation or reactions.
To avoid block pores or causing other problems from frequent emollient application, ensure you are applying in the direction of hair growth.
Steroid containing medicines applied to the skin are well tolerated and cause minimal effects when used in their short courses as prescribed.
If used for longer periods, or when short courses are often repeated, there is an increased likelihood of developing side effects including thinning of the skin.
What does infected Eczema look like?
Eczema causes skin to dry and break apart, so the risk of bacterial infection increases around the cracks. Excessive scratching or incorrect treatment regimens will further increase this risk. Typical symptoms of infected eczema include:
- Swelling and soreness
- Yellow discolourations on the flaked skin
- White or yellow spots on the affected skin
- Fluid or pus around the affected area
- Fever and other flu-like symptoms
Infections can cause existing symptoms to worsen, and prevent normal medication from being effective. You should consult your GP immediately if you notice that you or your child might have infected eczema.
Infections are typically treated with antibiotics and by ensuring the skin is clean and protected from further infection. When the infection has cleared, you will be required to switch to brand new creams, so as to prevent further contamination.
When using an emollient and a steroid, which one do you apply first?
You should apply the emollient first and allow it be absorbed.
Absorption usually takes around 10 - 15 minutes. When it is complete, the skin should feel slightly tacky to touch.
You are then ready to apply a thin layer of steroid cream.
What is the difference between the different steroid creams?
Corticosteroid creams vary based on their strength. Mild corticosteroids such as hydrocortisone can be purchased at pharmacies. You will require prescriptions for more potent types such as betamethasone dipropionate. Your GP will prescribe the lowest potency that will effectively combat your symptoms.
Do eczema scars go away?
Scarring from eczema is a common problem, as the intense itching can lead to scratching of the skin surface that results in bleeding and cracking. For many, this can lead to feelings of self-consciousness, especially if the scars are highly visible – on the arms, face, neck and legs, for example. The scars can range in colour and size, depending on their severity.
One of the best ways to prevent scarring is not to scratch. But this can be hard. Try using an anti-itch cream like E45 to reduce some of the intensity. If you already have visible scars, there are various good dermatitis creams available, and you should also aim to moisturise your skin often to keep it smooth and hydrated. Consult with one of our pharmacists here at The Independent Pharmacy to discuss which treatment is likely to be the most effective for your condition, whether you’re looking for relief or to minimise the visible damage and scarring of previous bouts of eczema.
What should I eat to help get rid of eczema?
There is no ‘wonder food’ that will totally cure you of the symptoms of dermatitis, but research has shown that certain changes to the diet can have a beneficial effect. Cutting out lactose – as found in cow’s milk – is one of the most common suggestions for eczema sufferers, and it is recommended that you try switching to a vegetable milk alternative to see whether this has any effect on your condition. Others have also suggested experimenting with cutting out foods such as gluten, eggs, soy, nuts, sugar and strong citrus fruits, to see if your condition could be partially related to an intolerance.
On the other hand, increasing consumption of foods like healthy fats (olive and coconut oils), grains and vegetables have been shown in some to have a positive effect. Essentially, any effort that can be made to follow a good, healthy, balanced diet may all help to improve health generally and relieve symptoms – alongside a good topical treatment to provide additional relief.
Eczema: how does it start, and what is it caused by?
Unfortunately, the exact cause of eczema is still unknown. It is generally considered to be the body’s way of overreacting to a certain irritant, which could be why some sufferers find the condition improves after eliminating certain foods from the diet. However, eczema also often runs in families (alongside asthma). It usually starts in areas such as the face, the back of the knees, wrists, hands or feet.
Atopic eczema is often diagnosed alongside very dry skin, where certain people have trouble retaining their skin’s moisture. For this reason, it’s important to moisturise regularly if you suffer with the condition – using an emollient shower gel is also recommended, as frequent showering under hot water can actually contribute to the drying effect.
Are there ways to treat eczema naturally?
Alongside the recommended creams and ointments, there are various other natural remedies that dermatitis sufferers claim help to relieve their symptoms – particularly certain kinds of oils. These include:
- Cod liver oil
- Coconut oil
- Jojoba oil
- Probiotics
- Sea spray
- Shea butter
- Oatmeal
- Chamomile
- Honey
- Witch hazel
It’s worth keeping a log to write down the effects of various remedies, to see what works and what doesn’t. Every one's skin is different and may react better to certain treatments that others.
Eczema and dermatitis: whats the difference?
To clear up the distinction, dermatitis is a term that refers to skin inflammation (hence the ‘itis’), whereas eczema is a more general term that applies to many types of dermatitis, but not all of them. So for example, atopic dermatitis would be considered a form of eczema, which could also include contact dermatitis, stasis dermatitis and neurodermatitis.
You can develop dermatitis without having eczema, for example, if your skin comes into contact with lots of stinging nettles and becomes inflamed, you could be said to have temporary dermatitis. Eczema sufferers can be said to be experiencing both.
Do allergies cause eczema?
Most of the time when eczema occurs, it’s not the result of an allergy. However, being around things that you are already allergic to can certainly exacerbate the condition considerably, if you are already experiencing eczema symptoms. This is because your body’s immune system is already in overdrive trying to fight off the irritant that’s causing the eczema in the first place.
Studies have shown that in children, if one or both parents have eczema, asthma or seasonal allergies, then the child is much more likely to be at risk. Indeed, it’s not uncommon for the three of them to occur together.